Penicillin is a type of antibiotic. It is used to treat infections in the body caused by some types of bacteria.1
Many people report being allergic to penicillin. However, the Centers for Disease Control and Prevention (CDC) states that fewer than 1 in 100 people who think they’re allergic to penicillin really are.2
If you think you’re allergic to penicillin—or aren’t sure—getting tested can give you the answer.2

of people in the United States—or 33 million Americans—report that they have a penicillin allergy2,3
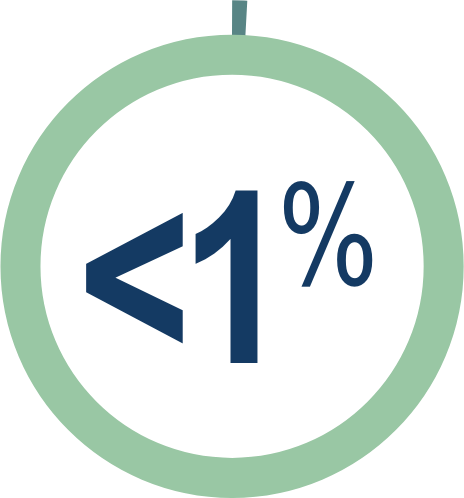
Yet according to the CDC, <1% of people who report having a penicillin allergy are actually allergic2
Why do so many people think they’re allergic?
Some of the reasons why someone might think they’re allergic to penicillin include1,2
1.
They had an allergic reaction to penicillin in the past.
Note: this can change over time, and many people may no longer be allergic.
2.
Sometimes, people mistake common side effects—such as an upset stomach—for a penicillin allergy. While this is a common side effect, it doesn’t mean they’re allergic.
3.
People can also mistake the symptoms of the infection that they are being treated for—or unrelated symptoms—as an allergic drug reaction.
About 4 out of 5 people with a penicillin allergy grow out of it within 10 years2
A true penicillin allergy can cause anaphylaxis (an-uh-fuh-lAk-suhs), which can be very dangerous and even life-threatening. When this happens, a person’s throat may start to close, it may be hard to breathe, and their blood pressure may drop.1
Why does it matter if YOU don’t really have a penicillin allergy?
Antibiotics are important tools in fighting bacterial infections. But every time we use them, there is a potential that the bacteria (or “bugs”) will start to become resistant. This is when the “bugs” create ways to defend themselves against an antibiotic, making it less effective.4,5
Narrow-spectrum antibiotics—like penicillin—target only the “bugs” known to cause a specific bacterial infection. Using these narrow-spectrum antibiotics whenever possible helps slow the development of antibiotic resistance.6,7
However, if penicillin is not an option due to a penicillin allergy, your doctor may need to use an antibiotic that treats many different bugs—commonly known as a broad-spectrum antibiotic. Because these drugs target a wider range of “bugs,” they increase the chances that resistance will develop.2,7
When antibiotics don’t work anymore, bacterial infections become harder to treat. This can mean more time in the hospital, more doctor visits, or a greater risk of spreading the disease.4
Facts about antibiotic resistance in the United States8
35,000
deaths are caused by antibiotic-resistant bacteria each year
2,800,000
infections are caused by antibiotic-resistant bacteria each year
How can you find out if you really are allergic to penicillin?
Your doctor can give you a simple skin test to see if you’re allergic to penicillin.2
For more information and resources about penicillin allergy, visit nationalpenicillinallergyday.com.
References: 1. Penicillin allergy. Mayo Clinic. Published December 5, 2019. Accessed June 24, 2021. https://www.mayoclinic.org/diseases-conditions/penicillin-allergy/symptoms-causes/syc-20376222 2. Evaluation and diagnosis of penicillin allergy for healthcare professionals. Centers for Disease Control and Prevention. Updated October 31, 2017. Accessed June 24, 2021. https://www.cdc.gov/antibiotic-use/clinicians/penicillin-allergy.html 3. U.S. and world population clock. Accessed June 24, 2021. https://www.census.gov/popclock 4. About antibiotic resistance. Centers for Disease Control and Prevention. Published March 13, 2020. Accessed June 24, 2021. https://www.cdc.gov/drugresistance/about.html 5. Antimicrobial resistance. World Health Organization. Published October 13, 2020. Accessed June 24, 2021. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance 6. Glossary. Narrow-spectrum vs broad-spectrum antibiotics. Alliance for the Prudent Use of Antibiotics. Accessed June 24, 2021. https://apua.org/glossary 7. Antibiotic treatment in the hospital: sometimes it can be stopped. American Board of Internal Medicine Foundation. Published February 2016. Accessed June 24, 2021. https://www.choosingwisely.org/patient-resources/antibiotic-treatment-in-the-hospital 8. Antibiotic resistance threats in the United States, 2019. Centers for Disease Control and Prevention. Accessed March 10, 2021. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf